Liver biopsy
Liver biopsy is usually performed in the liver to determine the type of the suspicious mass detected by imaging methods such as ultrasound, CT or MRI. More rarely, it is used to demonstrate the presence and degree of diseases such as hepatitis, cirrhosis, which involve the entire liver. The standard method used for these purposes is the cutting needle biopsy (trucut or core biopsy).
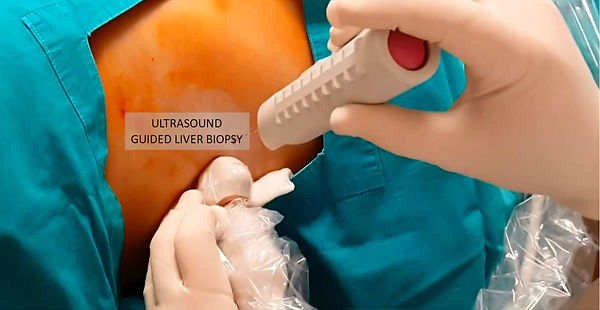
For trucut needle biopsy, a special needle is inserted from the skin under local anesthesia and ultrasound guidance, and small stripes of samples are removed from the mass. Fully automatic core biopsy needles automatically do this when a button is released. Tissue pieces are then placed in formaldehyde solution and sent for pathology examination.
Trucut or core needle biopsy is a safe and accurate biopsy method in liver as in other organs. During liver biopsy, major bleeding may occur in about 1% of patients. This risk may be increased if the target tumor is rich in vessels or if there are some factors that increase the risk of bleeding in the patient (such as low platelet count, liver dysfunction, blood thinner medications). In such cases, coaxial biopsy technique may be preferred. In this method, first the target tumor is reached with a separate needle, then the needle is held constant and a thinner trucut needle is inserted through this needle and several samples are taken from the mass. After that, the trucut needle is taken out and the bleeding is checked; If there is no bleeding, the external needle is withdrawn, if there is bleeding, some substances (coil, glue, patient's own blood clot, etc.) may be given through the external needle to stop the bleeding.
Video information: "Ultrasound guided liver biopsy"

Interventional oncology in cancer management
Prof Saim Yilmaz, MD


